What is intrauterine insemination? – Overview
Introduction:
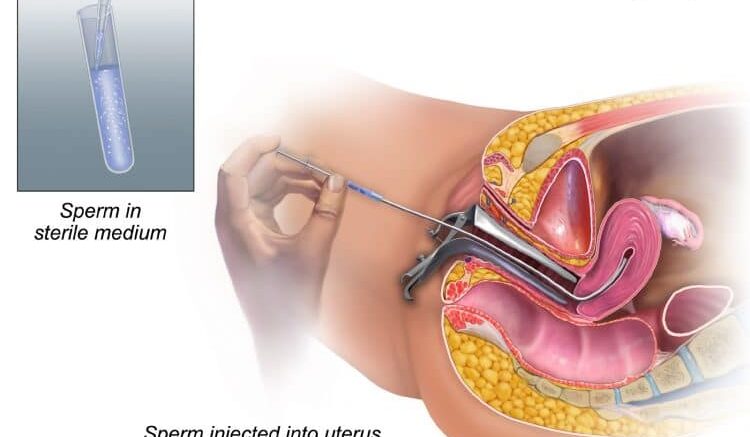
Intrauterine insemination is a type of artificial insemination that involves the direct placement of sperm into a woman’s uterus.
This process is highly recommended as a first-line treatment to treat unexplained infertility in both males and/or females. In this technique, sperms are ‘washed’ and ‘concentrated’ before directly placing them in the uterus (closer to the egg), which relatively permits a higher number of motile sperms to reach the egg and in turn, increases the chance of a normal pregnancy.
Sperm can be used by either your partner or a donor. Washing serves the purpose of removing any antigenic proteins, infectious agents, and prostaglandins.
It also removes any immotile sperms, leucocytes, and immature germ cells.
The sperms are concentrated in a small volume of culture media which is later inserted into the uterus through a transcervical catheter.
The procedure is simple to perform and at the same time, cost-effective and non-invasive.
A Brief History of IUI

What-is intrauterine insemination
The first case of human intra-vaginal insemination was described by John Hunter in 1770. Later on, in 1784, the first IUI was reported by Lazzaro Spallanzani which resulted in the birth of three puppies.
In the mid-1800s, 55 intravaginal inseminations were reported. Out of which only one pregnancy occurred.
In 1953, a simple method of preserving human sperm with glycerol was introduced and the first successful human pregnancy with frozen sperm was reported in the same year and was made public only a decade later.
The preference for IUI increased in later years and in 1988, 127 births in 20 clinics as a result of IUI with pre-treated serum were reported. In the decades of 2000, IUI had been used as a treatment option for cervical hostility, malefactor, and unexplained fertility.
IUI recently has gained wide popularity since it offers undeniable benefits.
Efficacy and Studies on intrauterine insemination:
Predicting the efficacy of IUI is difficult since every couple will have a different response.
The success rate of IUI largely depends on several factors: age, BMI, body weight, poor sperm or egg quality, severe case of endometriosis, severe fallopian tube damage or blockage, the underlying cause of infertility, and so on.
Studies are suggesting a 10-20% pregnancy rate per patient (on average), but that may range from as low as 5% to as high as 70%. Other research carried out in 2008-2015 showed an average pregnancy rate of 13% per cycle of IUI.
Various research studies suggest that IUI is highly cost-effective compared to other measures, like surgery, or in vitro fertilization.
The pregnancy rate can be further enhanced by simultaneously stimulating the ovary. Cumulative pregnancy rates of 19.7, 36.8, and 36.8% have been reported in 3 cycles of IUI in patients with a cervical factor, and pregnancy rates of 12.8, 29.3, and 38.3% for 3 cycles in couples with a malefactor.
Potential associated risks:
IUI comes with a few potential risks. The procedure is simple, non-invasive, and does not require anesthesia (painless). Some of the risks include:
- Mild cramps (similar to that in period)
- Slight risk of infection (0.01-0.2%) due to catheterization and injection of the semen specimen
- Ectopic pregnancies and spontaneous miscarriages may occur (this can also be observed in other infertility treatment modalities)
- Production of antiserum antibodies may occur
- Multiple pregnancies may occur
- When used along with ovarian stimulation, ovarian hyperstimulation syndrome may be seen
Who are the candidates for this and why is this done?
There can be multiple factors playing a role in or affecting pregnancy. Any person unable to conceive a baby normally would be the best candidate for Intrauterine insemination. IUI is mostly used by people:
- Unable to perform vaginal sex, either due to physical disability or psychosexual problem
- In a same-sex relationship and wish to conceive
- A single woman wishing to conceive
- Need specific help in conception
Both, males and females, diagnosed with unexplained infertility problems are good candidates. IUI helps to improve low sperm count or motility of sperm inside a female tract for increasing pregnancy chances. IUI may be helpful for males having infertility due to ejaculatory disorders.
Females diagnosed with mild endometriosis and/or those with unreceptive cervical mucus and anovulation are other good candidates.
Females of age 35 years or higher wishing to conceive also can opt for IUI.
IUI may not be effective for:
- Females with severe endometriosis
- Severe male factor infertility
- Females with blocked or removed fallopian tubes or with a severe fallopian tube disease
- Females with multiple pubic infections
- Males who do not produce any sperms (however, IUI may be performed using donor sperm)
Conclusion:
Intrauterine insemination is a simple, non-invasive, cost-effective, and relatively low-risk treatment that might work best for many females or couples trying to conceive.
It is the first-line treatment option for infertility due to cervical factors, anovulation, male factor, immunological factor, or unexplained fertility and females diagnosed with minimal endometriosis condition.
The procedure is painless and does not carry higher risks. A few side effects include the potential risk of infection and slight vaginal bleeding, ectopic pregnancy, or multiple pregnancies.
This technique can be a wonderful option for females or couples who have been struggling with normal conception.
References:
- Abdelkader, A. M., & Yeh, J. (2009). The Potential Use of Intrauterine Insemination as a Basic Option for Infertility: A Review for Technology-Limited Medical Settings. Obstetrics and Gynecology International, 2009, 1–11. https://doi.org/
- Aboulghar, M., Baird, D. T., Collins, J., Evers, J. L. H., Fauser, B. C. J. M., Lambalk, C. B., Somigliana, E., Sunde, A., Tarlatzis, B., Crosignani, P. G., Devroey, P., Diczfalusy, E., Diedrich, K., Fraser, L., Geraedts, J. P. M., Gianaroli, L., Glasier, A., & Van Steirteghem, A. (2009). Intrauterine insemination. Human Reproduction Update, 15(3), 265–277. https://doi.org/10.1093/
- Allahbadia, G. N. (2017). Intrauterine Insemination: Fundamentals Revisited. In Journal of Obstetrics and Gynecology of India (Vol. 67, Issue 6, pp. 385–392). Federation of Obstetric and Gynecological Societies of India. https://doi.org/10.1007/
- Cohlen, B., Bijkerk, A., Van Der Poel, S., & Ombelet, W. (2018). IUI: Review and systematic assessment of the evidence that supports global recommendations. In Human Reproduction Update (Vol. 24, Issue 3, pp. 300–319). Oxford University Press.
- Intrauterine insemination (IUI) – Mayo Clinic. (n.d.). Retrieved May 25, 2021, from https://www.mayoclinic.org/tests-procedures/
- Ombelet, W. (2017). The revival of intrauterine insemination: evidence-based data have changed the picture. Facts, Views & Vision in ObGyn, 9(3), 131–132. http://www.ncbi.nlm.nih.gov/pubmed/
- Starosta, A., Gordon, C. E., & Hornstein, M. D. (2020). Predictive factors for intrauterine insemination outcomes: a review. Fertility Research and Practice, 6(1), 1–11. https://doi.org/10.1186/